Overview
Hodgkin lymphoma, also called Hodgkin's disease, is one category of lymphoma, a cancer of the lymph system. When lymphatic cells mutate (change) and grow unregulated by the body's processes that normally decide cell growth and death, they can form tumors.
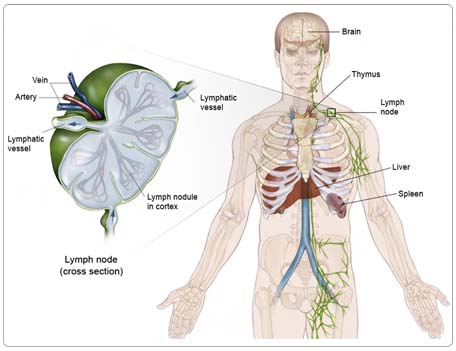
The lymph system is made up of thin tubes that branch out to all parts of the body. Its job is to fight infection and disease. The lymph system carries lymph, a colorless fluid containing lymphocytes (white blood cells). Lymphocytes fight germs in the body. B-lymphocytes (also called B cells) make antibodies to fight bacteria, and T-lymphocytes (also called T cells) kill viruses and foreign cells and trigger the B cells to make antibodies.
Groups of bean-shaped organs called lymph nodes are located throughout the body at different sites in the lymph system. Lymph nodes are found in clusters in the abdomen, groin, pelvis, underarms, and neck. Other parts of the lymph system include the spleen, which makes lymphocytes and filters blood; the thymus, an organ under the breastbone; and the tonsils, located in the throat.
Hodgkin lymphoma most commonly affects lymph nodes, usually beginning in the neck or the area between the lungs and behind the breastbone. It can also begin in groups of lymph nodes under the arms, in the groin, or in the abdomen or pelvis.
If Hodgkin lymphoma spreads, involvement of the spleen and liver is fairly common. Spread to other parts of the body can also occur, but it is unusual.
Risk Factors
A risk factor is anything that increases a person's chance of developing cancer. Some risk factors can be controlled, such as smoking, and some cannot be controlled, such as age and family history. Although risk factors can influence the development of cancer, most do not directly cause cancer. Some people with several risk factors never develop cancer, while others with no known risk factors do. However, knowing your risk factors and communicating them to your doctor may help you make more informed lifestyle and health-care choices.
The exact cause of Hodgkin lymphoma is not known, but the following factors may raise a person's risk of developing Hodgkin lymphoma:
Age. Hodgkin lymphoma occurs most often in people between the ages of 15 and 40 and in people over age 55.
Gender. Men are slightly more likely to develop Hodgkin lymphoma than women overall, although the nodular sclerosis subtype is more common in women.
Family history. Brothers and sisters of people with Hodgkin lymphoma have a higher chance of developing the disease (although the likelihood is still remote).
Virus exposure. People who are infected with EBV (see Overview) may be at increased risk for developing some types of Hodgkin lymphoma. However, there are probably several other factors involved. Mono is a very common disease, but Hodgkin lymphoma is very uncommon. For those cases not associated with EBV, other viruses may be involved.
It is important to note that although viruses may be involved in the development of Hodgkin lymphoma, there is no evidence that this type of cancer is contagious. Close contacts with someone with Hodgkin lymphoma does not increase a person's risk of developing the disease.
Symptoms
People with Hodgkin lymphoma may experience the following symptoms. Sometimes, people with Hodgkin lymphoma do not show any of these symptoms, or these symptoms may be caused by a medical condition that is not cancer. If you are concerned about a symptom, please talk with your doctor.
- Painless swelling of lymph nodes in the neck, underarm, or groin area that does not go away in a few weeks
- Unexplained fever that does not go away
- Unintended weight loss
- Night sweats (usually drenching)
- Itching
- Tiredness
If the lymph nodes in the chest are affected, they may press on the windpipe and cause shortness of breath, cough, or chest discomfort.
Diagnosis
Doctors use many tests to diagnose cancer and determine if it has metastasized (spread). Some tests may also determine which treatments may be the most effective. For Hodgkin lymphoma, a biopsy is the only way to make a definitive diagnosis. If a biopsy is not possible, the doctor may suggest other tests that will help make a diagnosis. Imaging tests may be used to find out whether the cancer has metastasized. Your doctor may consider these factors when choosing a diagnostic test:
- Age and medical condition
- The type of cancer
- Severity of symptoms
- Previous test results
In addition to a physical examination, the following tests may be used to diagnose Hodgkin's lymphoma:
Biopsy. A biopsy is the removal of a small amount of tissue for examination under a microscope. Other tests can suggest that cancer is present, but the diagnosis of Hodgkin lymphoma can only be made after a biopsy of an affected piece of tissue. Most commonly, this will be a lymph node in the neck, under the arm, or in the groin. If there are no lymph nodes in these areas, biopsy of other lymph nodes, such as those in the center of the chest, may be necessary.
This type of biopsy usually requires minor surgery, although occasionally it is possible to obtain a biopsy using a needle under local anesthesia, while the patient is undergoing a scan (most commonly a computed tomography [CT or CAT] scan, see below). The CT scan is used to help make sure the biopsy is taken from the appropriate place.
Treatment
The most common treatment methods for Hodgkin lymphoma are radiation therapy, chemotherapy, or a combination of both methods. Clinical trials of newer treatments may also be an option. Treatment choice will depend on the stage of the disease, the size of enlarged lymph nodes, the number of affected lymph nodes, the results of blood tests, the type of Hodgkin lymphoma, and the patient's age and general health.
Some of the original treatments for Hodgkin lymphoma, developed in the 1960s and 1970s, were very effective. However, long-term follow-up care of people who received these treatments has shown that they are at risk for late side effects including infertility (the inability to have children) and second cancers, such as lung cancer and breast cancer in women. These long-term problems were partly the result of the types of chemotherapy used at that time and partly the result of extensive radiation therapy.
To avoid or reduce the risk of these problems, modern treatment of Hodgkin lymphoma involves newer chemotherapy treatments and the use of much smaller fields of radiation therapy. Most patients with Hodgkin lymphoma, even stage I or stage II, will now be recommended to receive some chemotherapy, followed by radiation therapy to the affected lymph node areas. For stage III or stage IV disease, chemotherapy is still the primary treatment although additional radiation therapy may be recommended, especially to areas of large lymph nodes.
Radiation therapy
Radiation therapy is the use of high energy x-rays are used to destroy cancer cells and shrink malignant tumors.
Radiation therapy for Hodgkin lymphoma is always external-beam radiation therapy, which uses a machine to deliver x-rays to the site of the body where the cancer is located. As mentioned, whenever possible, radiation therapy is now typically targeted to the affected lymph node areas to reduce the risk of side effects.
Immediate side effects from radiation therapy depend on what area of the body is being treated. These may include mild skin reactions, upset stomach, loose bowel movements, nausea, and sore throat. Most patients feel tired. Many side effects can be helped with medication and usually go away when treatment ends.
Although the risk for long-term damage gets lower as treatments improve, radiation therapy may still sometimes cause long-term side effects, also called late effects. To minimize the risk of long-term side effects, clinical trials that seek to determine the best doses and smallest possible field for radiation therapy are being done.
Chemotherapy
Chemotherapy is the use of drugs to kill cancer cells. Systemic chemotherapy is delivered through the bloodstream, targeting cancer cells throughout the body. Many different types of chemotherapy may be used for Hodgkin lymphoma. The most commonly used combinations of drugs in the United States are called "ABVD" and "Stanford V." Another combination of drugs known as "BEACOPP" is now used widely in Europe and is being used more commonly in the United States.
ABVD: doxorubicin (Adriamycin), bleomycin (Blenoxane), vinblastine (Velban), and dacarbazine (DTIC). ABVD chemotherapy is usually given every two weeks for four to eight months.
Stanford V: mechlorethamine (Mustargen, Nitrogen Mustard), doxorubicin, vinblastine, vincristine (Oncovin), bleomycin, etoposide (VePesid), prednisone, and G-CSF (granulocyte colony stimulating factor). Chemotherapy is given weekly for two to three months and usually two to three of these drugs are administered each week.
BEACOPP: bleomycin, etoposide, doxorubicin, cyclophosphamide (Cytoxan), vincristine, procarbazine, and prednisone. The treatment schedule and number of cycles varies according to each patient's needs.
At the moment, it is unclear which of these chemotherapy treatments is best for patients with Hodgkin lymphoma, and the best treatment may differ according to the type and stage of the disease. For this reason, many clinical trials are underway comparing these different chemotherapy treatments. The clinical trials are designed to determine which combination is the most effective for the treatment of Hodgkin lymphoma and which has the fewest early and late side effects.
At various points during the course of chemotherapy, it is usual to have some of the original tests, especially CT scans and PET scans, repeated. These tests are used as a way to monitor the disease and to see how well it is responding to treatment.
Chemotherapy attacks rapidly dividing cells, including those in normal tissues such as the hair follicles, lining of the mouth, intestines, gonads, and bone marrow. Chemotherapy may cause patients to lose their hair, develop mouth sores, and have nausea and vomiting. Chemotherapy may also cause infertility, lower the body's resistance to infection, cause fatigue, and lead to increased bruising and bleeding. Other side effects may include numbness and tingling in the fingers and toes, loss of appetite, constipation, and diarrhea. The severity of the side effects depends on the type of drug used and how long it is taken.
Most side effects can be controlled during treatment with medication and usually go away after chemotherapy is completed. Although the risk of long-term damage from chemotherapy decreases as treatments improve, chemotherapy still sometimes causes late and permanent side effects.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications you've been prescribed, their purpose, and their potential side effects or interactions with other medications. Learn more about your prescriptions through PLWC's Drug Information Resources, which provides links to searchable drug databases.
Stem cell transplantation
Stem cell transplantation is a technique used to treat Hodgkin lymphoma with very high doses of chemotherapy to kill the lymphoma cells and then introduce new stem cells (that can form new blood cells) into the body. It is a difficult but relatively safe treatment and is reserved for patients with Hodgkin lymphoma whose disease is progressive or recurrent.
Stem cells are blood-forming cells that are usually found in the bone marrow. They can be collected and used for transplantation, either from the bone marrow in the hipbone or, more commonly, from the blood. If the stem cells come from the patient, it is called an autologous (AUTO) transplantation. If the marrow comes from another person, it is called an allogeneic (ALLO) transplantation.
In an AUTO transplant, stem cells from the bone marrow are first "mobilized" into the blood by treating the patient with chemotherapy and another drug known as G-CSF. The stem cells are then collected from the patient's blood, frozen, and stored. In an ALLO transplant, the donor stem cells are collected on or near the actual transplant day; the patient receives these fresh and unfrozen. Then, in both ALLO and AUTO transplants, the patient receives very high doses of chemotherapy (sometimes also with radiation therapy) to treat the Hodgkin lymphoma. These high doses are used since patients who undergo this treatment have disease that has proven to be resistant to normal chemotherapy doses. Higher doses of chemotherapy are more effective against recurrent Hodgkin lymphoma than standard doses of chemotherapy.
Although the patient's bone marrow may be severely damaged by this high-dose chemotherapy, the stem cells will be given to the patient after the high-dose therapy by means of an intravenous (IV) infusion and will restore blood cell production.
This type of treatment is now standard for patients with progressive or recurrent Hodgkin lymphoma (see below).
A mini-(non-ablative) transplantation is one that uses reduced intensity treatments before the transplantation. It is sometimes given to patients who may be too old or may not have the strength to go through the standard bone marrow transplantation process. This type of transplantation is being evaluated in clinical trials to determine its effectiveness in treating lymphoma.
Progressive or recurrent Hodgkin lymphoma
Progressive disease is when the cancer spreads while the patient is being treated. Recurrent means the cancer has come back after treatment. Progressive disease and recurrence are uncommon in Hodgkin lymphoma. If either occurs, most patients will be advised to receive high-dose therapy with a peripheral blood stem cell transplantation (see above), which appears to be more effective in treating progressive or recurrent Hodgkin lymphoma than another standard chemotherapy treatment.
Side Effects of Cancer and Cancer Treatment
Cancer and cancer treatment can cause a variety of side effects; some are easily controlled and others require specialized care. Below are some of the side effects that are more common to Hodgkin lymphoma and its treatments. For more detailed information on managing these and other side effects of cancer and cancer treatment, visit the PLWC Managing Side Effects section.
Diarrhea. Diarrhea means frequent, loose, or watery bowel movements. It is a common side effect of certain chemotherapy or radiation therapy to the pelvis.
Dry mouth (xerostomia). Xerostomia occurs when the salivary glands do not make enough saliva (spit) to keep the mouth moist. Because saliva is needed for chewing, swallowing, tasting, and talking, these activities may be more difficult with a dry mouth. Dry mouth can be caused by chemotherapy or radiation treatment, which can damage the salivary glands. Dry mouth caused by chemotherapy is usually temporary and normally clears up about two to eight weeks after treatment ends. Radiation treatment to the head, face, or neck can cause dry mouth. Fortunately, the radiation fields used for Hodgkin lymphoma only rarely include the salivary glands. It can take six months or longer for the salivary glands to start producing saliva again after the end of treatment.
Fatigue (tiredness). Fatigue is extreme exhaustion or tiredness and is the most common problem patients with cancer experience. More than half of patients experience fatigue during chemotherapy or radiation therapy, and up to 70% of patients with advanced cancer experience fatigue. Patients who feel fatigue often say that even a small effort, such as walking across a room, can seem like too much. Fatigue can seriously affect family and other daily activities, can make patients avoid or skip cancer treatments, and may even affect the will to live.
Hair loss (alopecia). A potential side effect of radiation therapy and chemotherapy is hair loss. Radiation therapy and chemotherapy cause hair loss by damaging the hair follicles responsible for hair growth. With chemotherapy, hair loss may occur throughout the body, including the head, face, arms, legs, underarms, and pubic area. The hair may fall out entirely, gradually, or in sections. In some cases, the hair will simply thin-sometimes unnoticeably-and may become duller and dryer. With radiation therapy, hair loss only occurs in the area being irradiated. Losing one's hair can be a psychologically and emotionally challenging experience and can affect a patient's self-image and quality of life. However, the hair loss is usually temporary, and the hair often grows back, especially after chemotherapy.
Infection. An infection occurs when harmful bacteria, viruses, or fungi (such as yeast) invade the body and the immune system is not able to destroy them quickly enough. Patients with cancer are more likely to develop infections because both cancer and cancer treatments (particularly chemotherapy and radiation therapy to the bones or extensive areas of the body) can weaken the immune system. Symptoms of infection include fever (temperature of 100.5° F or higher); chills or sweating; sore throat or sores in the mouth; abdominal pain; pain or burning when urinating or frequent urination; diarrhea or sores around the anus; cough or breathlessness; redness, swelling, or pain, particularly around a cut or wound; and unusual vaginal discharge or itching.
Mouth sores (mucositis). Mucositis is an inflammation of the inside of the mouth and throat, leading to painful ulcers and mouth sores. It occurs in up to 40% of patients receiving chemotherapy treatments. Mucositis can be caused by a chemotherapeutic drug directly, the reduced immunity brought on by chemotherapy, or radiation treatment to the head and neck area.
Nausea and vomiting. Vomiting, also called emesis or throwing up, is the act of expelling the contents of the stomach through the mouth. It is a natural way for the body to rid itself of harmful substances. Nausea is the urge to vomit. Nausea and vomiting are common in patients receiving chemotherapy for cancer and in some patients receiving radiation therapy. Many patients with cancer say they fear nausea and vomiting more than any other side effects of treatment. When it is minor and treated quickly, nausea and vomiting can be quite uncomfortable but cause no serious problems. Persistent vomiting can cause dehydration, electrolyte imbalance, weight loss, depression, and avoidance of chemotherapy. There are very effective drugs available to combat nausea.
Thrombocytopenia. Thrombocytopenia is an unusually low level of platelets in the blood. Platelets, also called thrombocytes, are the blood cells that stop bleeding by plugging damaged blood vessels and helping the blood to clot. Patients with low levels of platelets bleed more easily and are prone to bruising. Platelets and red and white blood cells are made in the bone marrow, a spongy, fatty tissue found on the inside of larger bones. Certain types of chemotherapy can damage the bone marrow so that it does not make enough platelets. Thrombocytopenia caused by chemotherapy is usually temporary. Other medications used to treat cancer may also lower the number of platelets. In addition, a patient's body can make antibodies to the platelets, which lowers the number of platelets.
After Treatment
After treatment for Hodgkin lymphoma ends, talk with your doctor about developing a follow-up care plan. Follow-up care after treatment for Hodgkin lymphoma is important for two major reasons:
- To monitor closely for possible recurrence (relapse) of the lymphoma
- To monitor for possible late side effects of treatment
This plan may include doctor visits and medical tests to monitor your recovery for the coming months and years. The frequency of follow-up care and the tests to be performed will depend on several factors, including the original extent of the Hodgkin lymphoma and type of treatment. Typically, all of the tests, including CT scans, PET scans, and bone marrow biopsies, will be repeated after treatment ends to ensure that there has been a complete disappearance of the disease. Then, additional scanning frequency will depend on the results of the initial set of tests.
In general, each follow-up visit will include a discussion with the doctor, physical examination, and blood tests. At some visits, scans will also be performed. At most cancer centers, follow-up visits are initially scheduled at two-month intervals during the time period with the greatest risk of recurrence, and the interval between visits is increased over time. Subsequent visits may only be two to three times per year until five years has passed; then, annual visits should be continued with an oncologist. Special attention will need to be paid to cancer screening and detection, as well as to cardiac (heart) risk factors, for the person's lifetime. For patients who received radiation therapy to the neck or chest, special attention to thyroid function will be important.
Follow-up care should also address the person's quality of life, including emotional concerns. In particular, Hodgkin lymphoma survivors are encouraged to be aware of symptoms of depression and promptly report them to their doctor.
Patients treated for Hodgkin lymphoma should get an annual flu shot. In addition, for certain patients, it will be recommended that they get an immunization against pneumonia, which may be repeated every five to seven years.
People recovering from Hodgkin lymphoma are encouraged to follow established guidelines for good health, such as maintaining a healthy weight, eating a balanced diet, engaging in regular exercise, and having recommended cancer screening tests. Talk with your doctor to develop a plan that is best for your needs. Moderate physical activity can help rebuild your strength and energy level. Your doctor can help you create an appropriate exercise plan based upon your needs, physical abilities, and fitness level.