The brain and spinal column make up the central nervous system (CNS), where all vital functions of the body are controlled. When a tumor arises in the CNS, it is especially problematic because a person's thought processes and movements can be affected. Also, this tumor can be difficult to treat because the tissues surrounding the tumor may be vital to functioning.
Anatomy of the brain
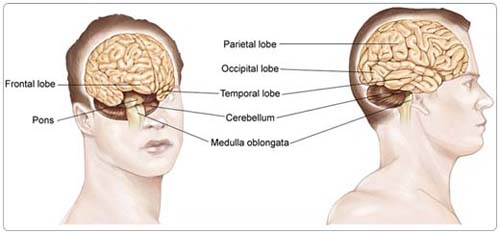
The brain is made up of:
The cerebrum, the largest part of the brain, contains two cerebral hemispheres and is divided into four lobes where specific functions occur:
- The frontal lobe, which controls reasoning, emotions, problem-solving, and parts of speech and movement
- The parietal lobe, which controls the sensations of touch, pressure, pain, temperature, and parts of speech
- The temporal lobe, which controls memory, sense of hearing, and parts of speech
- The occipital lobe, which controls vision
The cerebellum, or "little brain" is located beneath the cerebrum. The cerebellum is the back part of the brain responsible for coordination and balance. The brain stem, which is the lowest portion of the brain and connects to the spinal cord, controls involuntary functions essential for life, such as the beating of the heart and breathing.
The meninges are the membranes that surround and protect the brain and spinal cord. There are three meningeal layers, called the dura mater, arachnoid, and pia mater.
Types of brain tumors
There are more than 100 types of primary brain tumors. For a complete listing of their names and incidence, please refer to the Central Brain Tumor Registry of the United States. For practical purposes, this review is divided into glioma and non-glioma types of tumors.
Gliomas. Gliomas as a group are considered the most common type of brain tumor. A glioma is a tumor that grows from a glial cell, which is a supportive cell in the brain. There are two types of supportive cells: astrocytes and oligodendrocytes. Therefore, most gliomas are called either astrocytoma or oligodendroglioma, or a mixture of both. Gliomas are graded (how much the tumor appears like normal brain tissue) from I to IV based on their degree of aggressiveness. A grade I glioma is a benign (non-cancerous) tumor, while grades II through IV are tumors with an increasing degree of aggressiveness and are therefore considered increasingly malignant (cancerous) in potential.
Types of gliomas:
- Astrocytoma is the most common type of glioma, making up about 11% of the primary brain tumors. Astrocytomas begin in cells called astrocytes in the cerebrum or cerebellum. Glioblastoma multiforme (also called grade IV astrocytoma) is a very aggressive form of astrocytoma.
- Oligodendroglioma is a tumor that develops from cells called oligodendrocytes. These cells are responsible for producing the myelin (a substance rich in protein and lipids [fatty substances]) that surrounds nerves. Oligodendrogliomas make up about 4% of primary brain tumors.
- Brain stem gliomas begin in the glial cells in the brain stem.
- Ependymomas, which begin in the ependyma (the cells that line the passageways in the brain where cerebrospinal fluid [CSF] is made and stored), make up about 2% of primary brain tumors.
- Mixed tumors, which are composed of more than one of the glial cell types, make up about 1% of primary brain tumors.
Non-glioma tumors. Non-glioma tumors begin in other types of cells in the CNS, and are described as either benign or malignant.
- Meningioma is the most common primary non-glioma brain tumor, making up about 27% of such brain tumors. It begins in the meninges surrounding the brain and spinal column and is most often benign. Meningioma can cause significant symptoms if it grows and presses on the brain or spinal cord.
- Acoustic schwannoma (also called acoustic neuroma) is a rare tumor that begins in the vestibular nerve and is normally benign.
- Craniopharyngioma is a benign tumor that begins near the pituitary gland. These tumors are rare, making up less than 1% of all brain tumors.
- Medulloblastoma, which begins in granular cells in the cerebellum, is most common in children and is most often malignant. Medulloblastomas make up about 2% of all brain tumors.
- Primary CNS lymphoma is a form of lymphoma (cancer that begins in the lymphatic system) that starts in the brain and makes up about 2% of all brain tumors.
- The pineal and pituitary glands, located near the base of the brain, are the location of about 7% of all brain tumors.
About 5% of all brain tumors cannot be assigned an exact type.
Risk Factors
A risk factor is anything that increases a person's chance of developing a disease, including cancer. There are risk factors that can be controlled, such as smoking, and risk factors that cannot be controlled, such as age and family history. Although risk factors can influence disease, for many risk factors it is not known whether they actually cause the disease directly. Some people with several risk factors never develop the disease, while others with no known risk factors do. Knowing your risk factors and communicating with your doctor can help guide you in making wise lifestyle and health-care choices.
The risk factors for a brain tumor include:
Age. Children and older adults are two groups most likely to be diagnosed with brain tumors.
Gender. Men are generally more likely than women to develop gliomas, while women are more likely to be affected by meningiomas.
Home/occupational exposures. Occupational exposures to solvents, pesticides, oil products, rubber, or vinyl chloride may increase the risk of developing a brain tumor, although there is no scientific evidence to date. Black hair dye has also been researched as a potential cause of brain tumors, although the data remains inconclusive at this time.
Some genetic conditions. Some genetic conditions, such as von Hippel-Lindau disease, Turcot syndrome, or neurofibromatosis, increase the risk of developing a brain tumor. Genetic predisposition accounts for less than 5% of brain tumor cases.
Exposure to infections, viruses, and allergens. Infection with the Epstein-Barr virus increases the risk of CNS lymphoma. Several types of other viruses have been shown to cause brain tumors in experimental animal studies; however, more data is needed in order to determine if exposure to infections, other viruses, or allergens affect human brain tumor risk.
Electromagnetic fields. Electromagnetic fields, such as energy from power lines or from cell phone use, may or may not increase the risk of developing a brain tumor, as current research has shown conflicting results. At this time, more research is needed. Since the research is inconclusive, caution should be taken with children using cell phones while the brain is still a developing structure. The World Health Organization (WHO) recommends limiting cell phone use and promotes the use of a headset for both adults and children.
Race and ethnicity. In the United States, whites have higher rates of gliomas but lower rates of meningioma than blacks. The rate of malignant brain tumors in Japan is less than half the rate found in Northern Europe.
Ionizing radiation. Treatment with ionizing radiation (including x-rays) has shown, in some cases, to be a risk factor for brain tumors.
Head injury and seizures. Serious head trauma has long been studied for its relationship to brain tumors. Some studies have shown a link between head trauma and meningioma, but not one between head trauma and glioma. A history of seizures has long been associated with brain tumors, but because brain tumors can cause seizures, it is not known if seizures increase the risk of brain tumors, or if anti-seizure medication increases the risk.
Diet (N-nitroso compounds). Some studies of diet and vitamin supplementation seem to indicate that dietary N-nitroso compounds might influence the risk of both childhood and adult brain tumors. Dietary N-nitroso compounds may be found in some cured meats, cigarette smoke, cosmetics, and among other sources. However, additional research is necessary before a definitive link can be established.
Exposure to nerve agents. One study has shown that some Gulf War Veterans are at increased risk of brain tumors due to exposure to nerve agents; however, additional research is necessary before a definitive link can be established.
At this time, there are no known means of preventing a brain tumor.
Symptoms
People with a brain tumor often experience the following symptoms. Sometimes, people with a brain tumor do not show any of these symptoms. Or, these symptoms may be similar to symptoms of other medical conditions. If you are concerned about a symptom on this list, please talk with your doctor.
Symptoms of a brain tumor can be general (due to the pressure of the tumor on the brain or spinal cord) or specific (due to the interruption of the normal functioning of a specific part of the brain). Generally, a brain tumor is not diagnosed until symptoms begin.
General symptoms include:
- Headaches, which may be severe and may worsen with activity or in the early morning
- Seizures
- Personality or memory changes
- Nausea or vomiting
- Vision changes, such as blurred vision
Symptoms that may be specific to the location of the tumor include:
- Pressure or headache near the tumor
- Loss of balance and difficulty with fine motor skills (cerebellum)
- Changes in judgment, including loss of initiative, sluggishness, and muscle weakness or paralysis (frontal lobe of the cerebrum)
- Partial or complete loss of vision (occipital lobe of the cerebrum
- Changes in speech, hearing, memory, or emotional state, such as aggressiveness and problems understanding or retrieving words (temporal lobe of cerebrum)
- Altered perception of touch or pressure, arm or leg weakness on one side of the body, or confusion with left and right sides of the body (parietal lobe of the cerebrum)
- Inability to look upward (pineal tumor)
- Lactation, altered menstrual periods, and growth in hands and feet in adults (pituitary tumor)
Diagnosis
Doctors use many tests to diagnose cancer and determine if it has metastasized (spread). Some tests may also determine which treatments may be the most effective. For most types of cancer, a biopsy is the only way to make a definitive diagnosis of cancer. If a biopsy is not possible, the doctor may suggest other tests that will help make a diagnosis. Imaging tests may be used to find out whether the cancer has metastasized. Your doctor may consider these factors when choosing a diagnostic test:
- Age and medical condition
- The type of cancer
- Severity of symptoms
- Previous test results
Most brain tumors are not diagnosed until symptoms appear. The neuro-oncologist (a doctor who specializes in direct and indirect effects of neoplasms [abnormal tissue] on the nervous system) can use the patient's symptoms as clues to the location of the tumor. In addition to asking the patient for a detailed history and doing a physical examination, an oncologist or neuro-oncologist may order some of the following tests to determine the presence, and perhaps the type or grade, of a brain tumor. The most effective and common way to diagnose a brain tumor is with a magnetic resonance imaging (MRI) scan, although computed tomography (CT or CAT) scans are still used. Positron-emission tomography (PET) scans are generally used to gain more information about a tumor while a patient is undergoing treatment or if there is a recurrence (the cancer comes back after treatment). The primary way of determining the type of brain tumor is with a pathology report (lab results) following a biopsy or surgery. A biopsy is used in tumors that are inoperable. See below for more information.
Treatment
People diagnosed with a CNS tumor generally need to seek treatment as soon as possible. The pressure caused by a growing CNS tumor can cause severe symptoms, including a backup of CSF and problems with blood circulation, which can damage delicate nerves and deprive cells of nourishment.
Treating brain and spinal cord tumors can be difficult. The blood-brain barrier, which normally serves to protect the brain and spinal cord from damaging chemicals entering those structures, also keeps out many types of potentially beneficial chemotherapeutic drugs. Surgery can be difficult if the tumor is near a delicate portion of the brain or spinal cord. Radiation therapy can damage healthy tissue. However, research in the past two decades has improved the survival rates of patients with brain tumors. More refined surgeries, a better understanding of what types of tumors respond to chemotherapy, and precise delivery of radiation have resulted in a longer life span and better quality of life for patients with brain tumors.
Surgery
Surgery is the most common type of treatment for a brain tumor and is often the only treatment performed for a benign brain tumor. Even if the cancer cannot be cured, its removal can relieve symptoms if it is creating pressure on parts of the brain. There have been rapid advances in surgery for a brain tumor, including the use of cortical mapping and enhanced imaging devices to give surgeons more tools to plan and perform the surgery. For a tumor that is near the speech center, it is increasingly common to perform the operation under awake conditions. Typically, the patient is awakened once the surface of the brain is exposed, and special electrical stimulation techniques are used to locate the speech center and thereby avoid causing any damage while removing the tumor.
Surgery to the brain requires the removal of part of the skull, a procedure called a craniotomy. After the surgeon removes the tumor, the patient's own bone will be used to cover the opening in the skull. Gliadel wafers that deliver chemotherapeutic drugs (see below) require surgery to put the wafers in the tumor bed site. This may be done at the same time as a craniotomy.
In addition to removing or reducing the size of the brain tumor, surgery can provide a tissue sample for analysis. For some tumor types, the results of the analysis can help in showing if chemotherapy or radiation therapy will be useful.
Radiation therapy
Radiation therapy is the use of high-energy x-rays or other particles to kill cancer cells. Oncologists may use radiation therapy along with surgery to slow the growth of aggressive tumors. Radiation can be directed in the following ways:
The linear-accelerator machine provides external-beam radiation therapy from outside the body to target the tumor within the brain; this is becoming increasingly more precise with the addition of multileaf collimators (a device that restricts and confines the x-ray beam to a given treatment area).
In stereotactic radiosurgery, a computer assembles images from CT scans or MRI scans to locate the tumor and help direct the radiation. This may involve the use of an external head device to "marry" the patient's head/tumor location to the incoming radiosurgery beams.
Brachytherapy uses radioactive seeds implanted directly in the tumor site; however, this treatment technique is rarely used at this time for a brain tumor.
Radiation techniques
The following radiation techniques may be used:
Conventional radiation therapy. The treatment location is determined based on anatomic landmarks and x-rays. In certain situations, such as whole brain radiation therapy for brain metastases, this technique is appropriate. For more precise targeting, more elaborate techniques are required. Chemotherapy may be used in conjunction with this type of radiation therapy.
Three-dimensional conformal radiation therapy. Based on CT and MRI images, a three-dimensional model of the tumor and normal tissues is created on a computer. Beam size and angles are determined that maximize tumor dose and minimize normal tissue dose.
Stereotactic radiosurgery. Stereotactic radiosurgery involves delivering a single, high dose of radiation directly to the tumor and not healthy tissues. It works best for a tumor that is only in one area of the brain and certain benign tumors, but is also used for multiple metastatic brain tumors. There are three methods by which stereotactic radiosurgery is performed:
- A modified linear accelerator is a machine that creates high-energy radiation by using electricity to form a stream of fast-moving subatomic particles.
- A gamma knife is another form of radiation therapy that concentrates highly focused beams of gamma radiation on the tumor.
- A cyber knife is a robotic device used in radiation therapy to guide radiation to the tumor target-particularly targets in the brain, head, and neck regions.
Fractionated stereotactic radiation therapy. Radiation therapy is delivered with stereotactic precision but divided into small daily fractions over several weeks using a relocatable head frame, in contrast to the one-day radiosurgery. This technique is used for tumors located close to eloquent or sensitive structures, such as the optic nerves or brain stem.
Intensity modulated radiation therapy (IMRT). Radiation therapy is delivered with greater intensity or dose to thicker areas of the tumor and with less intensity to thinner areas of the tumor. This is accomplished by placing tiny metal leaves in the beam to reduce the intensity of the beam in order to customize the shape of the dose to the shape of the tumor.
All of these more elaborate techniques are designed to achieve greater precision and minimize the dose to the surrounding normal brain tissue. Depending on the size and location of the tumor, the radiation oncologist may choose any of the above radiation techniques. In certain situations, a combination of two or more techniques is appropriate.
Very young children (younger than 5) are not usually appropriate candidates for radiation therapy because of high risk of damage to their developing brains.
Chemotherapy
Chemotherapy is the use of drugs to kill cancer cells. The goal of chemotherapy can be to destroy cancer remaining after surgery, slow the tumor's growth, or reduce symptoms.
Although chemotherapy can be given orally (by mouth), most drugs to treat cancer are given intravenously. IV chemotherapy is either injected directly into a vein or through a thin tube called a catheter, a tube temporarily put into a large vein to make injections easier. Some chemotherapeutic drugs are better at going through the blood-brain barrier. Also, the oncologist may use intrathecal or regional delivery of chemotherapy agents, in which the drugs are injected directly into the CSF or into the tumor through a tiny tube. Gliadel wafers (see above) are another delivery method of the drug carmustine (BCNU), a less-toxic form of chemotherapy that has been approved by the U.S. Food and Drug Administration (FDA). Temozolomide (Temodar) is an oral chemotherapeutic drug that is well tolerated by most patients.
Since chemotherapy affects normal cells as well as cancer cells, many people experience side effects from treatment. Side effects depend on the drug used and the dosage amount. Common side effects include nausea and vomiting, loss of appetite, diarrhea, fatigue, low blood count, bleeding or bruising after minor cuts or injuries, numbness and tingling in the hands or feet, headaches, hair loss, and darkening of the skin and fingernails. Side effects usually go away when treatment is complete.
Rarely, certain drugs may cause some hearing loss. Others may cause kidney damage. Patients may be given extra fluid intravenously for kidney protection. The oncologist may also prescribe corticosteroids to reduce swelling and help to relieve symptoms.
Combination chemotherapy may also be used. For a malignant brain tumor, it is expected that a combination of treatments will be required. Typically, treatment begins with surgery, followed by radiation therapy, and then chemotherapy. In rare situations, the chemotherapy may come before the radiation therapy. In other situations, the chemotherapy is administered during the radiation therapy. The decision on what sequence to follow is made by the oncologist or neuro-oncologist.
The latest standard of care for patients with glioblastoma is radiation therapy with oral chemotherapeutic drug temozolomide (Temodar) at a reduced dose, followed by monthly doses of temozolomide after radiation therapy. The monthly doses continue until the doctor determines that the patient has had enough chemotherapy to remain stable or the cancer comes back.
Convection enhanced delivery (CED) chemotherapy is a new method that allows chemotherapy to be delivered more safely and effectively by pumping the therapeutic agent under pressure directly into the brain. The agent links only to receptors located on tumor cells. By targeting the tumor cells, CED helps conserve healthy brain cells and prevents adverse side effects commonly found in traditional systemic (full-body) chemotherapy delivery methods.
The medications used to treat cancer are constantly being evaluated. Talking with your doctor is often the best way to learn about the medications you've been prescribed, their purpose, and their potential side effects or interactions with other medications. Learn more about your prescriptions through PLWC's Drug Information Resources, which provides links to searchable drug databases.
Immunotherapy
There is an increasing effort to boost the immune system of patients in order to enhance their ability to fight the tumor. Different methods are being applied, such as the use of dendritic cells or the use of vaccines aimed against a specific molecule that is expressed on the surface of the tumor cells. Several studies are currently being tested throughout the country. Visit the Clinical Trials section for more information.
Advanced/recurrent brain tumors
If, in spite of initial treatment, the brain tumor does not go into remission (the temporary or permanent disappearance of symptoms) or if it recurs, patients can still receive care to manage the symptoms caused by the tumor. Symptom management is always important since the symptoms of a brain tumor can interfere with quality of life.
Since a brain tumor is so rare, it can be hard for doctors to plan treatments unless they know what has worked in treating other patients with a brain tumor. Clinical trials are research studies that compare the standard treatments (the best treatments available) with newer treatments that may be more effective. Investigating new treatments involves careful monitoring using scientific methods and all participants are followed closely to track progress.
Due to advances in research, new drugs are being created to combat brain tumors. Many of these new drugs are called "small molecules" or "molecularly targeted therapies" because they are small in size (and can therefore be taken orally) and/or can attack a specific molecule or target within the brain tumor cells. These new drugs are being tested either alone or in combination with standard chemotherapy.